The United States is the highest spender on healthcare per capita of any country in the world, by a significant margin. These costs are necessarily passed on to patients, which provides ample opportunity for organizations to offer services that help reduce unnecessary costs.
Kermit, a medical device spend management company, tracks physician spend within operating rooms while maintaining patient wellbeing. Founded in 2011 in Baltimore, Maryland, Kermit was formed to provide transparency to hospitals to better understand surgical spending. Its cofounders, two former medical implant sales representatives, and a business executive, initially provided consulting services to hospitals to help to control these costs.
One of Greater Baltimore’s Fastest Growing Companies
Surgical spending transactions are typically tracked on handwritten paper bills, with manual checks to confirm compliance. Because of the manual nature of this process, controlling costs were extraordinarily difficult. This norm is at least 50 years old and has been a staple in the surgical billing process. Despite this challenge, the Kermit platform provides an innovative and novel solution to managing spend. Initially anticipated to take 12 months and 10 developers to create, Kermit was developed in 9 months with just one developer. The success of their platform has made Kermit one of Greater Baltimore’s 50 fastest-growing companies.
The Baltimore Business Journal (BBJ) is the leading source for business news, data and networking for the Greater Baltimore region. Every year, the BBJ identifies the fastest-growing private companies based on average percent change in revenue over a three-year span. To place in their fast 50 is not only a significant honor, but also a testament the success of Kermit’s offering.
Rich Palarea, CEO & Co-founder of Kermit, joined Make/Shift to talk about the secret sauce behind their success.
From Consulting Expertise to a Technology-Enabled Service
Rich Palarea, CEO & Co-founder of Kermit, began his healthcare career in an unlikely place. Coming from previous roles in spend management within the supply chain industry, he cofounded Kermit with former medical device representatives John Owens and Jason Smith.

Kermit’s solution tracks surgical billing for physician preference items (PPI), specifically for those that involve an implantable medical device. PPI is the tools and devices that physicians use in their work, from gloves to high-tech equipment. Physicians are largely free to decide what they need to perform surgery. During surgeries, representatives from medical device manufacturers are present in the operating room to ensure that the surgeon has everything he or she needs and to explain the proper use of the instrumentation, among other responsibilities. This representative earns a commission for the sale, putting their interests at odds with hospital staff.
As Palarea explains, Kermit is “adjudicating all of the invoices that are being generated from that transaction.” By housing the hospital’s negotiated prices in the form of a pricing file and contract, Kermit can inform hospitals in real-time what is being paid on any particular surgery. In doing so, Palarea is creating partnerships between surgeons, supply chain executives, and financial executives to determine the most cost-effective methods of performing these surgeries.
Palarea describes that his team “likes to think of [Kermit] as a technology-enabled service.” Their work started as a consulting service, originally working directly with hospitals on methods of reducing medical device spend. With Mendix, Palarea built the Kermit platform based on his previous consulting experience.
“We’ve harnessed all of the power of low-code to bring an idea that we had, which is a consulting service, to life inside of our application in a very quick way.”
Kermit’s value lies in its ability to democratize the knowledge that has been hoarded in hospitals within different silos, centralizing this information for analysis. Bringing transparency to spend management is crucial to keeping costs down. Palarea’s people-centric solution focuses on taking tribal knowledge and disseminating that in a way that doesn’t require his physical presence, which would have proven difficult in the face of COVID-19.
Introducing a Disruptive Technology to Tech Laggards
Hospitals are notorious for being tech laggards. Justifiably so, as any risk they take with new technology could be life or death for its patients. As such, Palarea and his team were required to build Kermit in a way that minimizes risk.
Medical device companies have their preferred way of doing business, surgeons have their preferred way of interacting with partners, and executives have their preferred way of driving transparency and cost savings. These occasionally competing priorities are critical to maintain, and diverting from key stakeholders’ norms introduces challenges. Palarea says that he was faced with a tough question: “how do you think about aligning those interests? How do you think about managing change in an organization when you’re bringing software and consulting to bear that’s, quite frankly, disruptive to each of those parties?”
One of the priorities of a hospital CFO is to reduce operating costs. Palarea’s team has created a business model that aligns with these goals. Kermit’s pricing is based on a percentage of the costs that they can save the hospital, providing a low-risk commitment to adopting their ‘disruptive’ technology.
Digitizing and Mirroring Previously Broken Workflows
With multiple stakeholders and workflows to consider, Palarea was cautious about introducing a technology that would disrupt operating room procedures. As Palarea explains, “[Kermit] is trying to actually honor all of those stakeholders, they all play an important role, and also honor the existing workflows.” Each of these workflows is critical to a functioning operating room, making it necessary for Palarea and his team to mirror their processes rather than introduce new ones entirely.
“The adoption of low-code here has been quite instrumental for us, basically what [Kermit] is doing is mirroring broken workflows inside a hospital so that [they] don’t have to change [their workflows].”
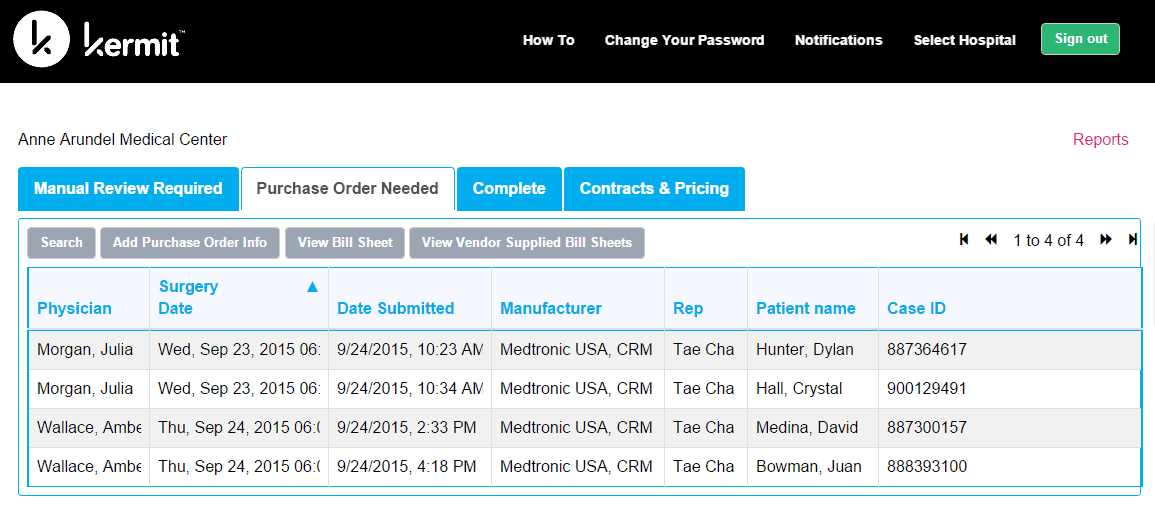
Many hospitals use pen and paper to track implants and the tools required for the surgeries. First, the paper they use to track implants turns into a requisition followed immediately by a purchase order. The purchase order is sent to the implant company, who generates an invoice to be sent back to accounts payable within the hospital. The paper process eventually transforms into an electronic transaction, but hospitals are still using outdated technology, like Electronic Data Interchange (EDI). These norms are error-prone and provide little visibility into the medical devices used by surgeons in operating rooms. As Palarea puts it, “when you start to collect this data [with Kermit], you can begin to illuminate all kinds of really interesting things going on.”
Kermit’s platform unlocks this antiquated technology and adjudicates in real-time without the need for human intervention. This helps to reduce the time that hospital executives are spending on vendor negotiations and provides unparalleled transparency into medical device spend. Forecasting and budgeting are more accurate, simplified, and based on real-time data.
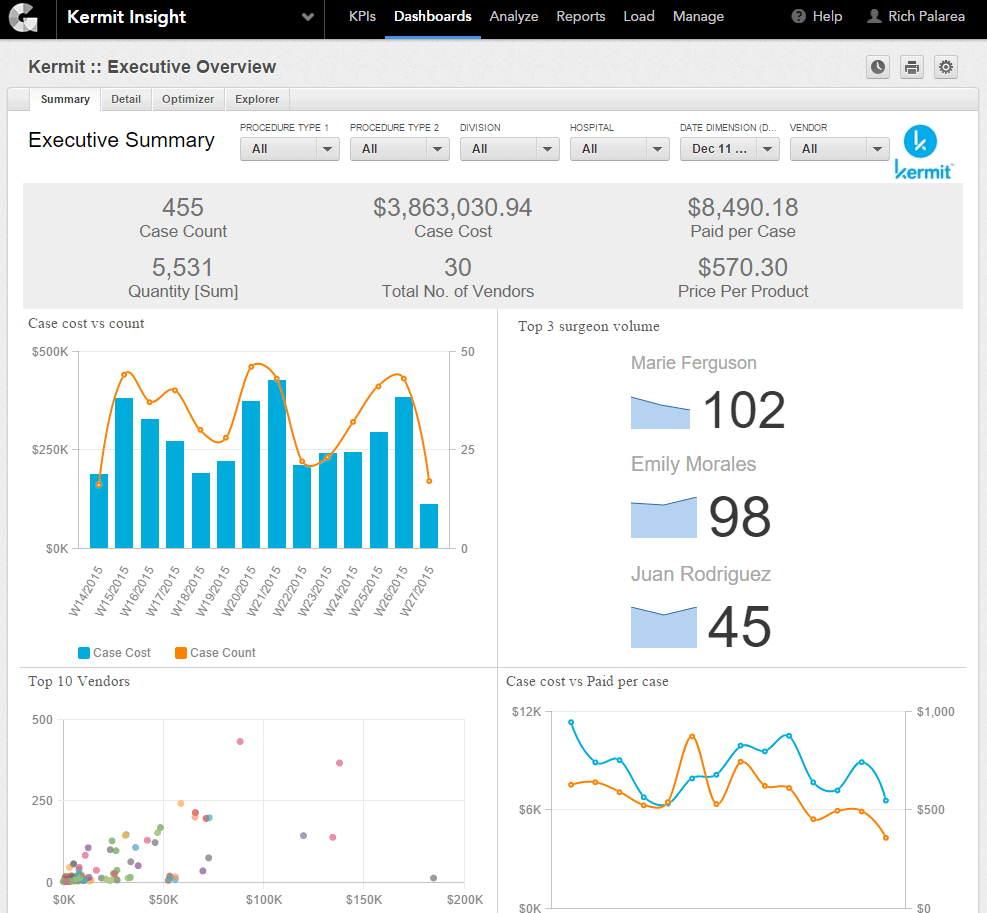
On top of auditing capabilities, their platform provides analytics comparing medical devices spend with patient wellbeing post-surgery. Palarea explains that “[Kermit] can find the intersection between getting the price down as low as possible, but still ensure that a patient has a fantastic outcome.” Hospitals can reduce costs without reducing positive results.
Avoiding the IT Juggernaut’s Concern Over HIPAA
Despite having buy-in from key stakeholders in the operating room and the executive suite, Palarea and his team always face one final obstacle to overcome – the IT department. Kermit handles patient data, which is very sensitive given the strict laws created by the Health Insurance Portability and Accountability Act (HIPAA). IT departments in hospitals are very concerned with any data that may fall under HIPAA, which pushed Palarea and his team to create a cloud-based solution.
“Kermit is self-contained in the cloud with all the security, and all the application layers, and all of the support that Mendix can provide to us to keep the system up and running with a very, very aggressive service level agreement that we can offer to the hospitals.”
Additionally, healthcare technology is typically expensive, complicated, and requires a significant implementation commitment. As Palarea explains, hospitals are “used to anywhere between a one- and three-year implementation, lots of customizations… [and] training for thousands of people.”
The implementation of their solution is simple. Once a hospital provides Palarea and his team with vendor contracts, pricing files, and a list of users, their instance can be stood-up in a single day. This is a breath of fresh air to the IT department, who shudder at the thought of introducing new software. In addition to passing security and HIPAA compliance audits, their platform does not need to be installed behind a firewall.
Kermit’s Healthy Future with Low-Code
During Kermit’s founding, Palarea recognized the amount of information that they were given access to. For example, it is necessary to collect specific lot numbers of implant devices to track medical spending. Even though his team didn’t have an explicit plan for leveraging this data, Palarea knew that if they held on to this data, they may understand where it may prove valuable.
During the COVID-19 pandemic, elective surgeries were ground to a halt. Palarea and his team looked to other ways to provide a valuable service to the patient population. Recognizing an opportunity to tie FDA recalls to their vast trove of data related to implant lot numbers, they realized they could offer a new service that notifies patients if their implant is subject to a recall. In addition to providing this new valuable service to patients, this allows hospitals to proactively manage recalled implants they may have administered. Insurance companies have indicated interest, enabling a wider range of industries that the Kermit platform appeals to.
Low-code has enabled Palarea to bring to market a solution that is reducing operating costs in hospitals while maintaining great patient outcomes. With Mendix, his team can trial different ideas, iterate quickly, and bring to market new products and services that drive additional business.

